This well-researched 2008 publication covers the concept of Alzheimer’s disease from its intriguing history to the monumental challenge it has become today. The book’s practical perspective provides a new lens by which to view the challenges of living with brain aging. Anecdotal sharing of my personal experiences of past and present will be interwoven into this review in order to describe why this book resonated for me.


Its release was ten years after I had relocated my office to my hometown to be with my parents in late 1998. I had sung daily with Mother during the entire period. It was a subject near and dear to my heart due to the joy and delight Mother and I derived together on a daily basis. During this experience, we soared!
The authors state that we need to hear about the unique stories to be found in this diagnosis. Instead, we continue to hear about the tragic “loss of self” – and other reductionist narratives.
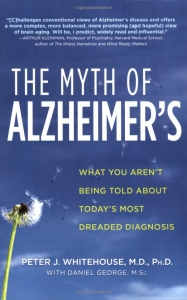
Returning from this appointment, I clicked into my Amazon account to order the first of two copies, which arrived the following day. Retrieving the book from the mailbox, I noted the lone dandelion in our flower bed at the mailbox – the only one on the entire lawn. It looked, mystically, like the one pictured on the cover of the book.
2008 – Trapped in Reductionist Framework
After reading the following in the Author’s Note, I knew I was definitely “on the same page.”
“Peter’s quarter-century in the field has convinced him that our entire approach to Alzheimer’s disease needs to change. The unique stories that people and families bring to old age cannot be captured by the simplistic and reductionistic framework of Alzheimer’s disease.” (p. vii)
Yes, I thought. Yes, exactly. The reductionist framework.
According to Dictionary.com, reductionism is “the practice of simplifying a complex idea, issue, condition, especially to the point of minimizing, obscuring, or distorting it. Simplistic. Oversimplified.”
During our rite of passage, we encountered our share of reductionism. It began on Day One.
Reductionism
The authors describe a phenomenally impersonal process in which people have all too frequently learned their diagnosis:
“Too often, aging patients and their families leave the doctor’s office with little more than a pill prescription (often encompassing several pills) and fear generated by the Alzheimer’s myth, knowing little about how to effectively care for the condition. . . This is inhumane and inexcusable.” (p. 6)
Reductionism – 1997-style: Over two decades have now passed since first learning of Mother’s diagnosis. But among the most vivid of memories is the day she was informed of her diagnosis.
She drove herself unaccompanied to her medical appointment. A neurologist who came to our hometown hospital from one of the regional medical centers on a weekly basis had made the diagnosis. A family representative was not informed of this appointment for which we would have been present – and for which, of course, we all needed to be present. She was alone and without any support when informed of this life-shattering diagnosis.
It is correct. She was given the handful of pills.
The authors would describe this diagnosis as one which imposed “too much unnecessary power” over her life. It was entered into her medical record – with finality: Alzheimer’s.
Stigma – from the major to the minor
Before we could put on our shoes – as the saying goes – the news of her diagnosis had traveled from our small town to halfway around the world. Their lives were changed forever – in every respect.
A powerful label had its grip upon us.
Soon, the side effects of her state-of-the-art pharmaceutical began to take a toll, sending Mother into a downward spiral. This was to be our first encounter with a near-death side effect being viewed as “the progression of her disease” and “the disease process.”
A reliable source would later reveal to me that my parents would return to the physician office in that first year on a frequent basis. Dad would definitely have persisted in his search to find the cause of Mother’s nausea. My parents could easily have been caricatured and dismissed by those working in the clinic – due to Dad’s persistence and their frequent return to the reception desk.
The medication causing the ongoing nausea and frequent return to the reception desk was Aricept. I could only wonder in the years which followed, “How long would you like to be nauseated? A day? A weekend? Daily for 13 months?”
Following my relocation – and after having quickly isolated the medication to be the cause of the nausea – I scheduled a follow-up consultation with the neurologist who had made the original diagnosis. It ran for close to one hour, during which time the physician chewed gum the entire hour of the consult. Annoying and unprofessional, it appeared to communicate his regard for us. Within the seclusion of his office – we were, it seemed, nonentities.
Binary pathways – 1998-2000
The locked unit had a detectable odor as we entered. It was obvious very quickly that Mother’s health status did not fit – in any respect – with the medicated residents lined up in a sphinx-like row.
As an articulate and independent woman, Mother would not fare well if confined in this bleak, deadly space. Who could? I knew deep in my being that, if admitted, it would be a matter of days until her actions and demeanor would match those around her. And Dad…? He would be admitted to a separate unit.
How could this be anything but abandonment of two people still full of life? Without any reservation, I believed that they needed support – not surrender and abandonment.
At what was still one of our early visits with the primary care physician, he quietly handed me a written physician order: “Nursing home admission.” I knew he was trying to help, but, quizzically, I wondered how recently he had stepped inside that unit.
Living proactively – celebrating interdependency
The mantras which prevailed in my head and heart included, “We’re not going to roll over and take it,” and, “It’s about dignity.”
By late 2000, after our move to “the ranch,” a modest duplex, we would live simply, but to our fullest abilities. We would stay together as long as we could all manage together. This was the unknown. Would it be for two months? Two years? Ten years?
For medical purposes, we used the label – Alzheimer’s – when speaking with medical personnel, in order to access every benefit due to Mother for this stigmatizing diagnosis. In reality, she received only one real medical “benefit” – the hospice experience provided in her final years.
Otherwise, we had no reason to even speak of “the label” or remind each other of any disability among us. We simply had no use for it. We were there to live our lives and be the best we could be. We would celebrate our interdependency and being together.
We would do our best to steer clear of rabbit holes and other distractions, but by this time it was abundantly clear that they covered the terrain.
Flashback to Dr. Alois Alzheimer – his unwitting legacy
Dr. Alois Alzheimer never personally called the condition a “disease,” but regarded it as “an effect of old age.” The authors state that Dr. Alzheimer himself had concluded that “there was no tenable reason to consider [his] cases as caused by a specific disease process.” (p. 100).
According to the authors, he died in 1915, unaware of his legacy.
The authors describe the diagnosis as “obscure” in the decades which followed – until the 1970’s when Alzheimer’s, as a “disease,” began to evolve as a “national institution.”
“One can only imagine how Alois Alzheimer … would have reacted had he been alive to see the enormous financial backing against a disease bearing his name in the latter decades of the twentieth century.” (p. 100).
The Alzheimer’s myth – an epidemic rolled out in the 1970’s
The authors point out that a diagnosis of Alzheimer’s “changes our relationship to those who are labeled with the disease. Instead of simply being persons with aging brains, they become ‘Alzheimer’s victims,’ diseased, demented, and stigmatized.”
So, if the person’s quality of life is not enhanced by using the state-of-the-art medication and being confined within a closed unit, then who benefits from the level of medicalization of this diagnosis?
The authors do not equivocate. From inside experience, they reveal big pharma’s role in the development of “Alzheimers the disease.” It has become a goliath from which big pharma benefits.
This publication is a comprehensive study of Alzheimer’s, laid out on a drawing board inviting our input. We all have a role in determining the future. How and where will we invest? Will it continue to be a future of darkness for many as dictated by the pharmaceutical industry? Or can we forge a future that leads to understanding, compassion and light? If we choose the latter, exactly how does that work?
The new story is about humanistic care.
The book created a huge shift in my universe – even after a decade of having been with my parents in a simple but always hopeful environment oriented to well-being.
The voices of Dr. Whitehouse and Dr. George were validating, scholarly, and yet practical – offering a holistic pathway to aging with dignity. With the contribution of their well-researched publication, leadership in the dementia community was gaining in strength and visibility. The publication appeared to elevate the national conversation.
Aging Well
When released, the title may have appeared provocative to some members of the dementia community. At a later date, however, the authors noted on their website that The Myth of Alzheimer’s had “aged well” in the intervening years.
As I page through my copy which is marked up with highlighting, asterisks, and red page tabs, I agree. I reflect on my own experience – and I am grateful to the authors for their leadership in describing a new, more humane future.
See “The Myth” Facebook page here. https://www.facebook.com/themythofalzheimers
Authors:
Peter Whitehouse, MD, PhD (Psychology) and MA (Bioethics)
Daniel George, PhD, MSc
______________
Author: Susan Troyer





Leave A Comment